‘Health’ is a term with a wide outlook. It may be interpreted distinctively and respectively by individuals. There is no single or precise definition as such to define health. Everybody has a different meaning and extent attached to it. For some being healthy would be in physical terms that is external in nature whereas for others being healthy would mean having a stable emotional and mental state. According to (WHO P. t., 1946) “Health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”
Health is a broad concept and has various dimensions – physical, emotional, mental, social, spiritual, intellectual, and environmental. Physical health can be viewed in terms of a person’s height, weight, age, blood pressure, and heart rate. Emotional health is a person’s ability to deal with feelings of joy, fear, sadness, anger, disgust, and surprise. Indicators of poor emotional health could be low mood, loss of appetite, nervousness, social anxiety, low energy, and sleeping problems. Mental health is a state of mental well-being where you feel to have peace of mind with the ability to think and actualize your highest potential. Spiritual health develops through meditation, in philosophy, it refers to the unity of body, mind, and soul. It results in increased focus and having a goal orientation outlook toward work and every aspect of our life. Intellectual health is the capability to apply critical thinking in activities that require mental effort. Thus health in areas of life is crucial for a person’s growth, productivity, and overall well-being.
Relation between Health and Productivity
“India is one of the most populated countries in the world and has a large human capital. Its Demographic Dividend will peak around 2041, when the share of working-age, i.e. 20-59 years, the population is expected to hit 59% according to an economic survey 2018-2019.”(Drishti ias, 2022)
Population acts as a resource for any country, if people residing in the country are making the best use of their abilities and skills therefore that population is considered to be productive and is an asset. But certain preconditions are required to be fulfilled to have such a resourceful population and one such precondition is health. Health is man’s greatest possession, investment in health means investment in human resource development which ultimately results in the development of a nation. Good health of citizens indirectly implies good production and efficient output with an increase in GDP(gross domestic country). Therefore a Healthy population is highly crucial for having steady growth and prosperity in any country.
A healthy population is a wealthy population if not taken care of and can soon turn into a liability from an asset. This makes health an important factor for the overall progress of a nation. Also, Health is something which is very much influenced by its environment and acts as an input for having good health. Environment and health go hand in hand and are highly interlinked and interdependent. Our environment consists of things that directly affect our lifestyles like proper sanitation and sewage system, clean drinking water, adequate housing, nutritious food, and free and compulsory primary education. All these are necessities that are required to be fulfilled to lead a healthy life and it is the sole responsibility of the Government to provide us with such an environment. The government must provide its citizens with a quality life and to do so a proper healthcare framework and a developmental plan were required. This led to the emergence of policymaking in the health sector within India.
Challenges of Healthcare in India
Numerous obstacles come in the way while dealing with the health care services and facilities in a developing country like India. Due to the country’s socio-economic condition, people face various hurdles in availing the healthcare facilities to which they are entitled. Some of them are as follows:
Lack of infrastructure, communication, and poor connectivity specifically in remote areas results in deprivation of access to proper sanitation and health care facilities. they don’t have well-equipped tools, technology, and well-educated doctors.
Secondly, the increase in the cost of medications and treatment these days has made even basic healthcare needs unaffordable for people below the poverty line, especially those with no health insurance. Thus poverty is a major challenge for healthcare today.
Thirdly, Differences in the Quality of healthcare provided by the healthcare workers. It may vary based on infrastructure, facilities available, nature, training, and practice of workers.
Fourthly, Inadequate use of Information and communication technology and advanced machines in dealing with healthcare. It is essential to get precise results and ensure better treatment.
Fifth, Chronic diseases such as diabetes, heart disease, and cancer are increasingly prevalent, and managing these conditions can be complex and expensive. There is a need for better prevention and management strategies to improve outcomes and reduce costs.
Sixth, As the population ages, there is an increasing demand for healthcare services, especially for older adults with complex medical needs. Providing appropriate care for this population can be challenging, especially as healthcare resources become more limited.
Lastly, A healthcare system operates best in the hands of healthcare workers. They are primarily responsible for executing day-to-day administrative activities and thus are indispensable assets for the smooth functioning of hospitals and healthcare systems. Inadequate spending on education and training of healthcare workers and mismanagement of employment strategies are major reasons for the continuous shortage of the workforce in the healthcare system.
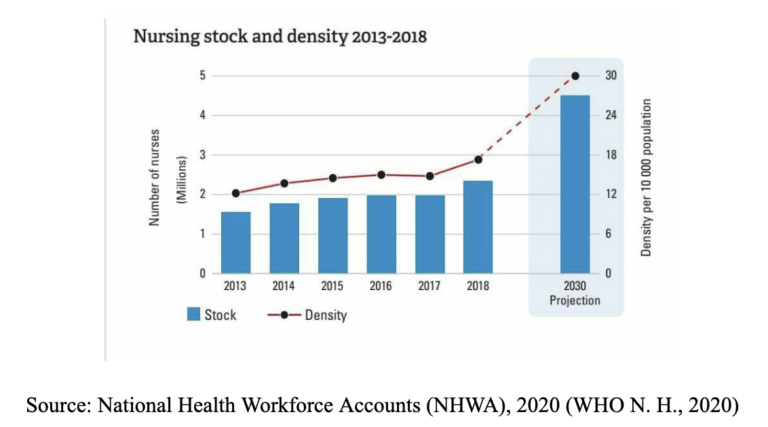
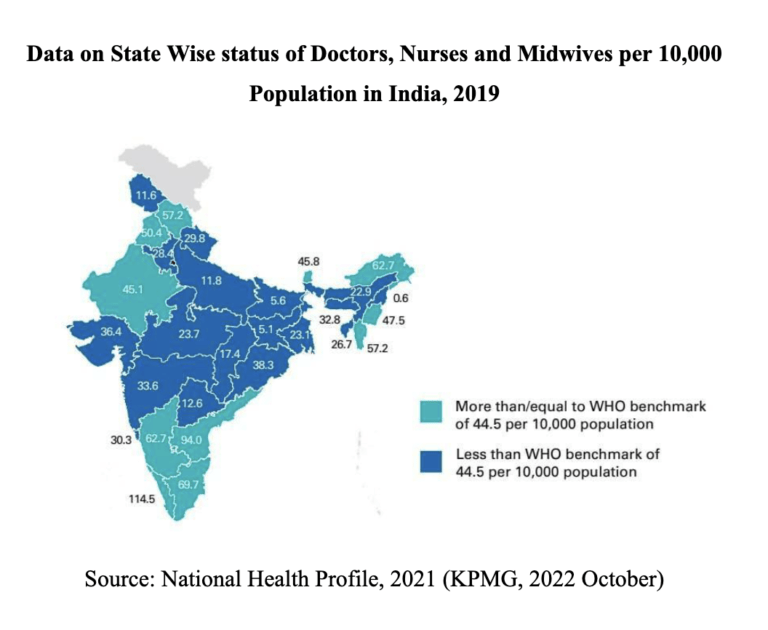
According to the data presented by NHWA in Figure 1 “ the density of nurses per 10,000 population has increased from approximately 2 million since 2013 to 3 million in 2018 and it is projected that it is likely to skyrocket by nearly 5 million in the year 2030. In addition, a recent WHO report also mentions that India needs at least 1.8 million doctors, nurses, and midwives to achieve the minimum threshold of 44.5 health workers per 10,000 population in 2030. (WHO, Decade for health workforce strengthening in SEAR 2015–2024, mid-term review of progress., 2020)”.
“Despite this increased recognition of the central role of the health workforce in attaining health outcomes and enhanced economic growth, the investment in the health workforce, particularly in lower and middle-income countries (LMICs) is lower than desired levels for education and training for health workers and ensuring health worker accessibility. (WHO, Global Strategy on Human Resources for Health: Workforce 2030, 2019)”
Moreover, according to the data presented in the Global Strategy on Human Resources for Health: Workforce 2030, WHO estimates a projected shortfall of 10 million health workers by 2030, mostly in low- and lower-middle-income countries. (WHO, Global strategy on human resources for health: Workforce 2030, 2020).
In addition, the advent of the COVID-19 pandemic consequently resulted in the shortage. Healthcare workers themselves got affected when they came into contact with patients of covid positive even after taking precautions. Exposure to the deadly virus followed by the quarantine of many healthcare workers, particularly in areas that have been hardest hit.
As a solution, recently in 2019, the government of India announced three strategies to enhance the supply of HRH:
(i) establishing new institutions to produce health workers; (ii) expanding the intake capacity of the existing medical institutions and (iii) upgrading existing district hospitals to the medical college level. (Schemes., 2021)
Furthermore, the advent of Covid 19 pandemic has led to an increase in the demand for healthcare workers and created a wide gap between the number of workers available and required. Thus leading to a shortage of workforce.
Structure and Composition of Human Resources for Healthcare in India
Our country’s healthcare system is a synthesis of traditional and Western medical practices. It includes allopathy, homeopathy, and ayurvedic treatments. Allopathy involves using scientific measures, clinical trials, heavy drugs, and surgical tools, whereas homeopathy is based on the composition of medicines using natural substances. Ayurveda is considered a gift of Indian heritage to the world’s healthcare systems. It includes age-old practices of meditation and yoga as a cure to many problems, specifically the ones currently affecting the upcoming millennials.
Healthcare professionals are classified into a wide range of variety contributing different domains in the system. Their role and responsibilities vary depending on their position. These go on to include Physicians, nurses, pharmacists, dentists, medical researchers, etc.
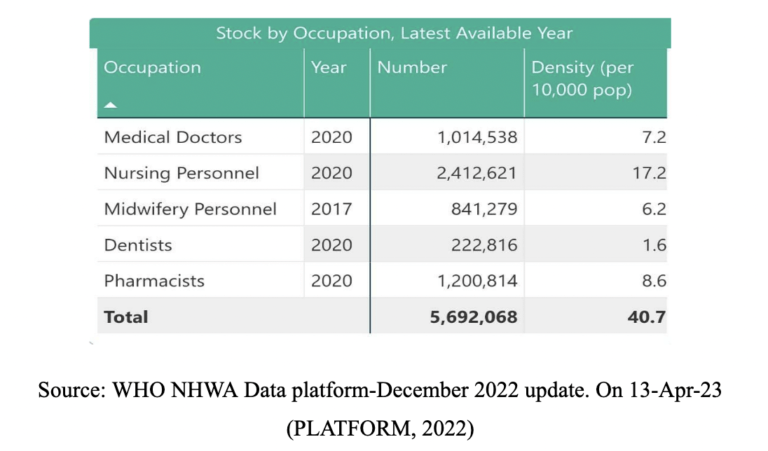
As per the latest data presented by NHWA in figure 2, the total stock of health care professionals based on their occupation available is 5,692,068, including 1,014,538 medical doctors, 2,412,621 nursing personnel,841,279 midwifery personnel,222,816 Dentists, 1,200,814 pharmacists.
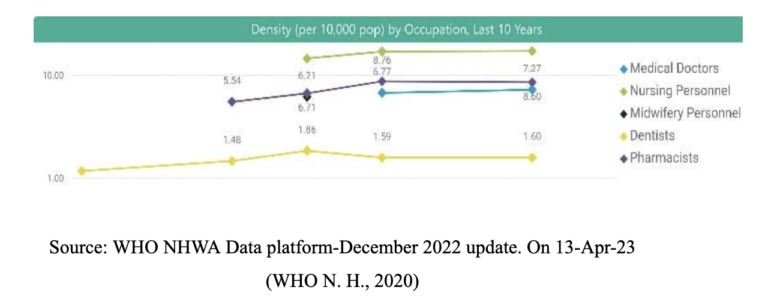
Furthermore, figure 3 depicts the occupational density of healthcare professionals as of 2020. The density of medical doctors per 10,000 population is 7.27, 17.28 nursing personnel, 6.21 midwifery personnel (2017), 1.60 dentists, and 8.60 pharmacists.
Future Estimates of Skilled Healthcare Workers
According to estimates provided by NSSO in Figure 5, The projected skilled health workforce numbers will rise from current estimates of 1.77 million to 2.65 million in 2030. However, even this will not result in a rise in the skilled health workforce density as the density will be approximately 17.5 per 10,000 population in 2030. There will be a shortfall of approximately 1.13 million skilled health workers to reach 22.8 skilled health workers per 10,000 population. However, if there is a scale-up of nursing supply to approximately 200% growth by 2030, the resultant number of nurses will be 2.02 million in 2030 and the total skilled health workforce number will be 3.45 million in 2030 (22.76 skilled health professionals per 10,000 population). (Anup Karan, 22nd March 2021)

Recommendations to Improve Our Healthcare System
Various committees have been formulated to provide suggestions to improve healthcare services and initiate policy reforms, Some of these are:
- Increasing the number of doctors and medical colleges: This would involve expanding medical education programs, as well as incentives to encourage more people to pursue careers in medicine.
- Developing new training programs and expanding existing ones will skill the unskilled workers which will result in better implementation and realization of needs in the healthcare system.
- Changes in nursing education programs to better prepare nurses for the evolving healthcare landscape, as well as policies to improve job opportunities and working conditions for nurses.
- Increased investment in training programs for paramedics and other allied healthcare workers, as well as policies to improve their working conditions and job opportunities.
- Have financing mechanisms to support the healthcare workforce, such as grants, loans, or tax incentives for healthcare providers.
- Combining of infrastructure, faculties, and facilities of different units into one for accreditation can result in better outcomes and boost healthcare
- To have a national platform that would include representatives from the private sector, development sector, professional bodies, and healthcare workforce in policy planning. Such a platform can provide a space for stakeholders themselves to share their perspectives, concerns, and suggestions regarding healthcare policies and workforce development. This will cater to future needs and better formulation of policies in the health sector.
- Have an e-portal for healthcare human resources that would facilitate in-hand access for both recipients and providers of healthcare services. The Portal would inculcate Certification courses for AHW Continuous learning/ Up-skilling, Training material Job portal, Inputs for the Robust Healthcare Skilling Platform, and bookings for appointments with doctors.
- Companies and private enterprises should be bound to provide a certain amount of funds for the better training and improvisation of healthcare sectors as a part of CSR initiatives
- Providing incentives to healthcare workers is imperative to keep them motivated to contribute, play their part and become fully committed to their respective jobs. Incentives can be a driving force to encourage healthcare trainees and workers to continue to pursue such fields.
- Being a part of the healthcare system, providing them extra social benefits like free medical insurance, accident risk potential, and free medical facilities for their family members.
- Increase in the use of digital technology and ICT in dealing with nursing, laboratory examinations, sample blood testing, and other medical equipment to get accurate reports. This will make our healthcare more advanced and up-to-date.
- Therefore, an inclusive, evidence-based, and tailored approach is required to improve our healthcare system and it is essential to meet up the WHO-recommended thresholds of 2030.
Role of the Covid-19 Pandemic
Covid 19 pandemic was declared a public health emergency of international concern by WHO. The COVID-19 pandemic has placed unprecedented pressure on health systems’ capacities, particularly health workforces. The impact of the epidemic was devastating on the world and exposed many loopholes in healthcare systems across the globe.
The first wave of the pandemic was certainly manageable, but the second wave proved to be much more challenging due to the shortage of beds, health care workforce, and essential medical supplies like oxygen cylinders. Schools and railway compartments were converted into makeshift treatment centers due to a shortage of hospital beds. The shortage of medical supplies also led to medicine being sold on the black market at exorbitant prices, putting additional financial strain on patients and their families.
India had a little more than 1.5 million isolation beds across 15,375 dedicated treatment facilities for a population of 1.38 billion. That translates to a skosh of over 1 bed per 1,000 people. Just 18% of these were oxygen-supported beds, according to the 2020-21 annual report of the Ministry of Health and Family Welfare. (Edwin, 2021)
Additionally, the lack of IT infrastructure in hospitals like AIIMS and Safdarjung made it difficult to maintain accurate data on patients, their treatments, and outcomes. This lack of information made it harder for healthcare workers to effectively manage patient care during the pandemic.
Overall, the COVID-19 pandemic has highlighted the need for robust healthcare systems that can respond to crises effectively. Governments and healthcare organizations must work together to address the issues that have been exposed to the pandemic and take steps to ensure that we are better prepared for future health emergencies.
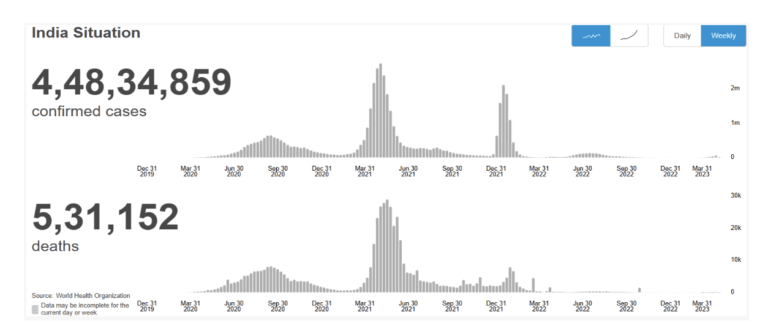
Data on the Covid-19 Pandemic
In India, from 3 January 2020 to 11:04 am CEST, 19 April 2023, there have been 4,48,34,859 confirmed cases of COVID-19 with 5,31,152 deaths, reported to WHO. As of 10 April 2023, a total of 2,20,66,24,273 vaccine doses have been administered. (World Health Organization (Covid-19) Homepage, 2022)
Overall, urgent actions are needed to achieve the target of having an additional one billion people enjoying UHC(United Health Coverage) by 2030. Based on current trends, approximately 730 million people will miss out on UHC; if the effects of the COVID-19 pandemic and its disruptions are taken into account, that shortfall could rise to 840 million. – (WHO, World Health statistics 2022, 2022)
Post-Covid Era
After the emergence of the first two waves of the covid 19 virus, the aftermath was followed by the upcoming of the ‘omicron virus’ which was a mutant virus of Sars Covs-2. It did not have much serious impact and was evadible with the effect of vaccination administered during the first and the second waves.
Recently, new trends like the ’XBB’ variant are considered to be a sub-variant of omicron coming up from the synthesis of BA.2.10.1 and BA.2.75, which are sub-lineages of the Omicron variant of Covid19.
A comparison of sequences submitted during weeks 44 and 45 shows an increase from 23.1% to 27.3% for BQ.1 and its descendent lineages. As of 28 November, BQ.1 has over 30 descendent lineages (BQ.1*). During the same period, the prevalence of XBB and its descendent lineages increased from 2.7% to 3.8%. BA.2.75 increased from 5.4% to 6.6%, while BA.4.6 decreased from 3.1% to 2.9%. BA.2.3.20 remained relatively stable at 0.4% in both weeks. (Organization, 30th November 2022)
On 20th April, a meeting was chaired by PM Narendra Modi to review the covid 19 situation in the country due to the rising number of cases. Focus was to evaluate the preparedness of health infrastructure, logistics, drugs, and vaccination drives in the country. As a part of the preparedness strategy drills are being conducted in the hospitals and the availability of essential commodities like drugs is being arranged in advance to tackle the loopholes faced earlier and avoid any kind of aggravating situation.
Eight states were given a status of high alert having a rise in the number of cases being reported namely, Kerala, Delhi, Maharashtra, Haryana, Uttar Pradesh, Tamil Nadu, Karnataka, and Rajasthan.
Moving forward, continued efforts to control the spread of the virus, increase vaccination rates, and address the social and economic impacts of the pandemic will be critical in mitigating its ongoing effects.
Allocation of Budget for the Healthcare Sector
An increase in the budget for the health sector has been seen in the 2022-2023 budget keeping in mind the necessity of spending to deal with the pandemic and its aftermath effects.
In 2023-24, the Ministry of Health and Family Welfare was allocated Rs 89,155 crore. (Welfare, 2023) This is an increase of 13% over revised estimates for 2022-23. The Department of Health and Family Welfare has been allocated Rs 86,175 crore, which accounts for 97% of the Ministry’s expenditure. (Research, 2023 Feb)
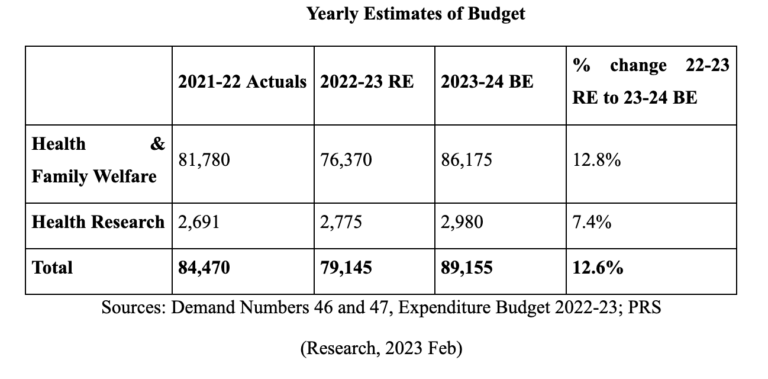
Between 2012-13 and 2023-24, allocation towards the Department of Health and Family Welfare increased at an annual average rate of 12%. The allocation increased from Rs 25,133 crore in 2012-13 to Rs 86,175 crore in 2023-24 (research, 2023 Feb).
Additionally, the government has also announced various schemes and initiatives aimed at improving the healthcare system in India, such as the Ayushman Bharat Scheme, which provides health insurance coverage to economically vulnerable populations of our society.
Conclusion
To conclude, in recent years, there has been growing recognition of the need to address systemic issues in healthcare and to promote a more patient- centred, equitable, and sustainable approach to healthcare delivery. Achieving these goals will require ongoing efforts and collaboration among healthcare providers, policymakers, patients, and other stakeholders.
References
Anup Karan, H. N. (22nd March 2021). Size, composition, and distribution of health workforce in India: why, and where to invest? BMC-Human Resource for Health.
drishtiias. (2022, December 24). Unlocking India’s Demographic Potential. Retrieved from https://www.drishtiias.com/daily-updates/daily-news-editorials/unlocking-india-s-demographic-potential/print_manually
Edwin, T. (2021, april 30th). Analysis: India has long been short of hospital beds. The pandemic intensified the shortage. Money Control is a pro.
KPMG. (2022 October). Strengthening healthcare workforce in India: the 2047 agenda. KPMG.
Organization, W. H. (30th November 2022). COVID-19 Weekly Epidemiological Update. WHO.
PLATFORM, W. N. (2022, December). National Health Workforce Accounts Data Portal. Retrieved from National Health Workforce Accounts Data Portal: https://apps.who.int/nhwaportal/Home/Index
research, P. l. (2023 Feb). Demand for Grants 2023-24 Analysis Health and Family Welfare.
Schemes., M. O. (2021). Establishment of New Medical Colleges attached to existing District/Referral hospitals. Ministry of Health and Family Welfare, Government of India.
Welfare, D. O. (2023). Ministry of Health and Family Welfare. Retrieved from Union Budget 2023-24: https://www.indiabudget.gov.in/doc/eb/sbe47.pdf
WHO. (2019). Global Strategy on Human Resources for Health: Workforce 2030. Geneva: World Health Organisation.
WHO. (2020). Decade for health workforce strengthening in SEAR 2015–2024, the mid-term review of progress. World Health Organisation.
WHO. (2020, July 7th). Global strategy on human resources for health: Workforce 2030. Retrieved from World Health Organization: https://www.who.int/publications/i/item/9789241511131
WHO. (2022). World Health Statistics 2022. World Health Organization.
WHO, N. H. (2020, march 10th). National Health Workforce Accounts. Retrieved from https://apps.who.int/nhwaportal/Sown/Files?name=IND
WHO, P. t. (1946, June). International Health Conference, New York, 19–22 June 1946. Retrieved from https://www.who.int/about/governance/constitution
World Health Organization (Covid-19) Homepage. (2022). Retrieved from WHO: https://covid19.who.int/region/searo/country/in